Blood Thinners and Oral Surgery
Blood thinners are a type of medicine that prevents your blood from clotting inside a blood vessel, which can lead to a heart attack or stroke. They can also keep blood clots from forming or getting larger. They are typically used to treat certain types of heart disease, heart defects, or other medical conditions that could increase your risk of developing blood clots.
A side effect to taking blood thinners is the difficulty to stop bleeding. This needs to be considered before any dental procedures take place. Always inform your dentist if you are taking a blood thinner medication, especially if you’ve just started one. It will be noted in your chart, and your cardiologist or other specialist will be consulted if you require a dental procedure with the potential for increased bleeding.
Precautions
Most general dental procedures, including teeth cleanings, fillings, and crowns, will not be affected if you are taking blood thinners. The only time an issue could arise is during an invasive surgery that has the potential to cause bleeding, such as a tooth extraction or gum surgery. Because the blood thinners don’t allow the blood to clot normally, stopping the bleeding during either of these procedures may be difficult.
After you’ve informed your dentist about which type of blood thinner you’re taking and the exact dose, and after consulting with a specialist, your dentist may suggest temporarily stopping or reducing your medication as a precaution. Other precautions may be taken, such as using hemostatic agents during your procedure to encourage blood clotting at the operation site, or being careful to suture the site to avoid hitting smaller blood vessels that can easily bleed.
Returning to Normal
If your medication was temporarily stopped or the dosage reduced for a dental procedure, you will be able to resume your blood thinners soon after the procedure is complete. It’s important to keep an open line of communication with your dentist, surgeon, and doctor. By all of you working together, your health will be at a much lower risk and your dental procedure will take place without complication.



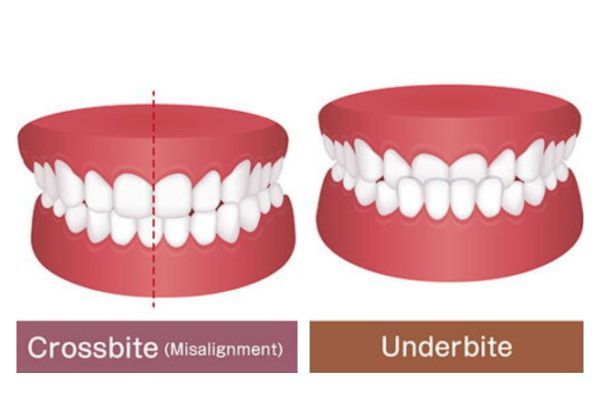


 Overbite
Overbite