Root Canal FAQs
What is a root canal?
The roots of your teeth have small openings, called root canals, which allow blood vessels and nerve fibers to bring nutrients and sensation to your teeth. If infection occurs in or around these small openings, it can damage the pulp inside of the tooth.
A root canal treatment is a procedure that removes damaged pulp from inside the tooth, and protects it from future infection.
Why do I need a root canal?
If tooth pulp becomes acutely inflamed or infected, it needs to be removed in order to save the tooth.
Pulpal damage is commonly caused by:
- Physical trauma, like a sports injury, that impacts the teeth
- Tooth decay (like a cavity) that advances into the root canal. Bacteria reaches into the pulp and nerve endings, causing infection, decay, and extreme sensitivity
- Broken teeth that expose the pulp to bacteria
Symptoms include:
- Tooth pain while chewing
- Tooth sensitivity to temperature
- Swollen gums or face
- Discolored or gray teeth
Is there an alternative?
The only alternative is to have a tooth extraction, which isn’t recommended because extraction can cause problems like teeth shifting position, difficulty chewing, and loss of jawbone density.
Root canal treatment has a 98% success rate, and can heal the tooth for a lifetime.
Is a root canal treatment painful?
A root canal treatment is done under local anesthesia, and might feel very similar to getting a filling.
What will happen during the procedure?
First, the affected area is numbed, and a dental dam is placed around the tooth to keep it dry during the procedure. A small opening is made at the top of the tooth and small tools are used to take out the infected pulp. Then the tooth is disinfected and filled with an inert, biocompatible material, and sealed with adhesive cement.
What will happen afterwards?
Pain and sensitivity might last for a few days after treatment, and can be relieved with over-the-counter medication like ibuprofen. You might be instructed to avoid chewing on the affected tooth for a few days. After a few days, the temporary filling is removed and replaced with a permanent filling or crown.
How can I avoid the need for root canal treatment?
You can prevent the need for root canal treatment by brushing and flossing every day, and scheduling regular cleanings. Acidic beverages, like soda, and sugar can contribute to infections in the mouth, so it’s best to avoid them. If you’re active in sports, it’s best to wear a mouthguard to protect your teeth from injury.





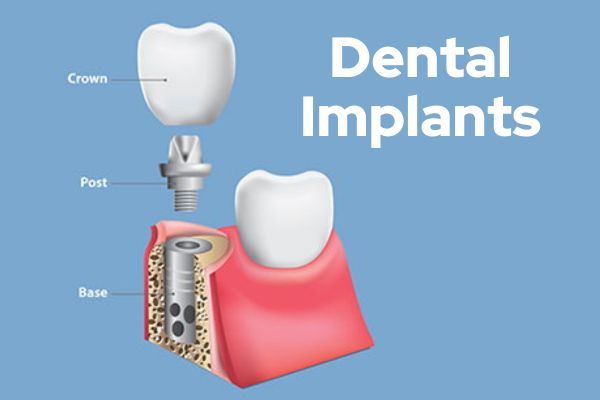

 If you are missing an entire arch of teeth due to injury or disease, whether it’s your lower or upper arch, it is possible to replace that arch with implant dentures. Implant-supported dentures are dentures fixed to the gums by mini implants. For patients with an uncomfortable or loose-fitting denture, stabilizing it with mini implants can be a more comfortable and functional solution. Implant dentures are the preferred choice over removable dentures because they look and act just like natural teeth, they don’t fall when you’re eating or talking, they prevent bone loss in your jaw, and they last a very long time.
If you are missing an entire arch of teeth due to injury or disease, whether it’s your lower or upper arch, it is possible to replace that arch with implant dentures. Implant-supported dentures are dentures fixed to the gums by mini implants. For patients with an uncomfortable or loose-fitting denture, stabilizing it with mini implants can be a more comfortable and functional solution. Implant dentures are the preferred choice over removable dentures because they look and act just like natural teeth, they don’t fall when you’re eating or talking, they prevent bone loss in your jaw, and they last a very long time.